Know Your Numbers | Make a Plan with Your Health Care Provider | Measure and Monitor at Home | How to Measure Blood Pressure
If you have a diagnosis of high blood pressure, a family history of it, or are proactively managing your health, monitoring your blood pressure helps you stay on track and prevent serious cardiovascular events. High blood pressure ranks as the top risk factor for stroke and a major risk factor for heart disease, dementia, and kidney failure. Known as the ‘silent killer’ because it often shows no symptoms, high blood pressure can go unnoticed for years without proper monitoring—yet, you can manage it effectively.
We suggest using this easy three-step strategy for optimal blood pressure management and monitoring.
Step 1: Know your numbers
Step 2: Make a plan with your health care provider
Step 3: Monitor
Fast Facts on blood pressuring monitoring at home:
- Home blood pressure, if done correctly using an approved devices2, is a better predictor of future cardiovascular risk than in-office blood pressure.
- Blood pressure monitoring frequency is dependent on many factors, such as is the degree of blood pressure elevation, the presence of other risk factors, and medication usage. In general, you should monitor more frequently if your blood pressure is not controlled, you have diabetes or cardiovascular disease, or if you are on medication.
- Studies have found that up to 80% of the at-home blood pressure monitoring devices used in the world are inaccurate! A list of Canadian approved monitors can be found here.
STEP 1: KNOW YOUR NUMBERS
High blood pressure often shows no signs. Many people don’t know they have it and its risks. Checking your blood pressure is the only way to know if you have it. Knowing your baseline blood pressure numbers is the first step to control it.
Understanding Blood Pressure Readings
Blood pressure has two numbers. The top number, systolic pressure, measures pressure when your heart beats. The bottom number, diastolic pressure, measures pressure when your heart rests.
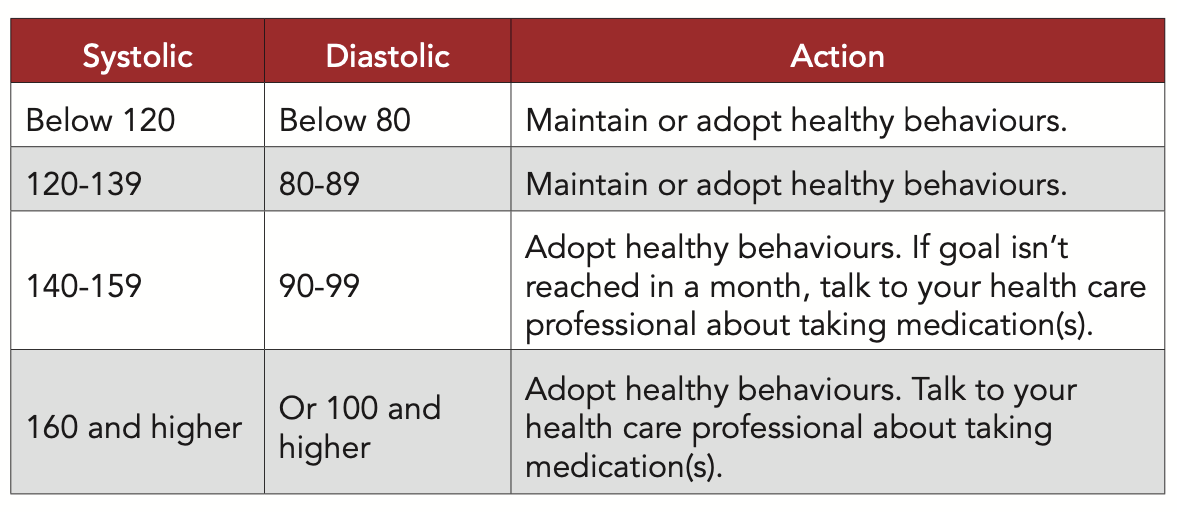
A chart can show normal and high blood pressure stages. Higher systolic or diastolic pressures mean more damage to blood vessels and organs. If your systolic pressure exceeds 180 mmHg or your diastolic pressure exceeds 120 mmHg, consult a health care provider immediately.
Guidelines for blood pressure categories can differ by country, with some exceptions. For instance, people with diabetes should aim for a blood pressure below 130/80 mmHg to avoid complications. Aging can naturally increase blood pressure due to stiffer arteries. Discuss your target blood pressure with your health care provider.
Did you know?
If you bring your blood pressure down the damage done to your arteries can be repaired over time. Similar to how the lungs of a once smoker can repair themselves, arteries can do the same!
Did you know?
Having diabetes raises the risk of heart disease, stroke and kidney disease. High blood pressure also increases these risks! If you have both high blood pressure and diabetes, your blood pressure target is typically lower for this reason. Many of the diet and lifestyle changes that can lower blood pressure can also lower blood sugar and reduce your risk of both!
STEP 2: MAKE A PLAN WITH YOUR HEALTH CARE PROVIDER
Your numbers and risk factors allow you to safely and effectively reduce your blood pressure and risk through several treatment options. Your unique case dictates the appropriate treatment, which might include changes in diet and exercise or multiple medications. You should actively collaborate with your healthcare provider to develop an individualized plan.
Your plan with your health care provider should include:
- Current blood pressure number
- Your target blood pressure number
- A detailed treatment plan, including one or all of the following: diet and lifestyle changes, medications, natural health products
- A blood pressure monitoring schedule, including how often should you be monitoring, and how to monitor
- A timeline for when you need to re-assess your plan
It is essential to openly communicate with your health care provider about medications, lifestyle factors, and any alternative treatments you use to control your blood pressure. As an important member of your health care team, you and your provider should work together as partners towards a common goal.
You should always inform your health care provider about any natural health care products you use, as they can interact with some medications. This allows your provider to confirm the safety of your treatment.
Always communicate the following to your health care provider:
- All blood pressure readings you have taken yourself including the date and time. You can use a phone application such as an app to record all of your readings. Using an app allows you to flexibly calculate averages and better understand your numbers. You can also use a printable blood pressure monitoring log like the one found here
- All medications you are on, the dose, and how often you take them
- All natural health care products you are on, the dose, and how often you take them
- Any changes to your signs and/or symptoms or any changes to your treatment plan
Did you know?
Many of the risk factors that increase blood pressure can be modified and lead to significant reductions alongside medications or supplements. Some of these risk factors include:
- Being overweight or obese
- Too much salt (sodium) in your diet
- Not being physically active
- Drinking too much alcohol
As you can imagine, the more risk factors you have the higher the likelihood your blood pressure is elevated. The opposite is also true! As you reduce your risk factors, your blood pressure should reduce accordingly!
Did you know?
Any changes to your treatment should always be communicated to your health care provider. When certain blood pressure medications are stopped there can be a rebound effect where blood pressure elevates even higher. This is a dangerous situation that can be avoided with proper communication.
STEP 3: MONITOR
Monitoring your blood pressure is a key step in managing it over time. Patients can actively participate in their care through home blood pressure measurements (HBPM) with validated devices, ideal for tracking treatment effectiveness and enhancing adherence. Ambulatory blood pressure monitoring (ABPM), requiring a 24-48 hour wearable monitor, is useful for detecting fluctuations, especially at night. However, we’ll focus on HBPM, as ABPM requires medical supervision.
Why monitor blood pressure at home?
Heart & Stroke Canada recommends all patients with high blood pressure monitor at home to determine if their treatment is effective. Tracking blood pressure at home is not a substitute for office visits with your health care provider but provides additional information to guide treatment.
Research has found that monitoring blood pressure at home is a better predictor of future cardiovascular risk than in-office measurement if done correctly and with an approved device2. Home blood pressure monitoring has also been found to significantly reduce both systolic and diastolic blood pressure and increase the number of individuals who can reduce their antihypertensive medication3. One study even found that patients who regularly monitored their blood pressure were 4 times more likely than those who didn’t monitor regularly to have controlled their blood pressure levels4!
How often should I be monitoring my blood pressure?
Several factors influence how often you should monitor your blood pressure: your current blood pressure levels, the presence of other risk factors like diabetes, and any recent changes to your medication. Your healthcare provider will collaborate with you to establish the right frequency for monitoring.
When measuring your blood pressure at home it is recommended that you take your blood pressure twice in the morning and twice in the evening. Taking these measurements before eating is preferred.
How do I properly monitor my blood pressure at home?
Ensuring at-home blood pressure measurements are done accurately and with approved devices is very important so you are not overly or under medicated.
Detailed instructions on how to monitor your blood pressure properly from home can be found here.
High blood pressure can be prevented, managed, and even reversed by knowing your numbers, having a plan and monitoring blood pressure regularly. Remember, hypertension is not a disease, it’s simply a signal that your body needs some cardiovascular TLC!
References
- Musa-Veloso, K., Paulionis, L., Pelipyagina, T. and Evans, M. (2019). A Randomized, Double-Blind, Placebo-Controlled, Multicentre Trial of the Effects of a Shrimp Protein Hydrolysate on Blood Pressure. International Journal of Hypertension, [online] 2019, pp.1-13. Available at: https://www.hindawi.com/journals/ijhy/2019/2345042/.
- McGrath, B. (2015). Home monitoring of blood pressure. Australian Prescriber, [online] 38(1), pp.16-19. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4654038/ [Accessed 24 Oct. 2019].
- George, J. and MacDonald, T. (2015). Home Blood Pressure Monitoring. European Cardiology Review, [online] 10(2), p.95. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6159400/ [Accessed 24 Oct. 2019].
- Kim, J., Han, H., Song, H., Lee, J., Kim, K. and Kim, M. (2010). Compliance With Home Blood Pressure Monitoring Among Middle-Aged Korean Americans With Hypertension. The Journal of Clinical Hypertension, [online] 12(4), pp.253-260. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4517578/.
Subscribe & Save
Two tablets. Every day. A lifetime of health.
Consistency is the key to maintaining healthy blood pressure levels and supporting your heart health. By taking two PreCardix® tablets every day, you’re building a daily routine that promotes long-term cardiovascular wellness and vitality.
Important Information
Always consult with your healthcare provider before making changes to your blood pressure management plan. PreCardix® does not treat, cure, or prevent medical conditions. Measure and monitor blood pressure regularly. Know the signs of heart attack and stroke.
Do not take PreCardix® if you are under age 18, if you are pregnant or breastfeeding, have renal artery stenosis, have a history of angioneurotic edema, or have a shellfish allergy. Consult product guidelines for additional information. Print and share the product monograph with your healthcare provider.
PreCardix® is an innovation of Marealis Inc. a Norwegian Bio-Tech company dedicated to finding natural, sustainable, and effective marine-based solutions for blood pressure health, globally. Designed in Norway. Manufactured in Canada.